Local emaciation refers to focal wasting or thinning of subcutaneous fat and muscle in a specific region of the body. Unlike generalized emaciation—where weight or muscle loss is systemic—local emaciation often springs from discrete causes such as nerve injury, repeated injections, or pressure atrophy. This comprehensive, evergreen guide explores the mechanisms, risk factors, clinical presentation, workup, management, and prevention of local emaciation, arming patients and clinicians alike with clear, evidence‑backed insights.
Introduction
Imagine a patient who notices a sunken area on one thigh after months of repeated injections—this is local emaciation in action. Though the overall body mass index remains stable, the affected region appears markedly thinner, impacting both function and appearance. Understanding local emaciation is crucial for timely diagnosis and targeted management, reducing long‑term disability and improving quality of life.
Understanding Local Emaciation
Definition & Pathophysiology
Local emaciation involves selective loss of adipose tissue, muscle fibers, or both in a confined anatomical zone. It arises when local metabolic demands, innervation, or mechanical forces disrupt normal tissue maintenance.
Generalized vs. Localized:
Generalized emaciation (cachexia, anorexia) affects the entire body.
Localized emaciation strikes one region, often unilateral.
Common Sites:
Thighs, buttocks (injection‑related).
Forearms (nerve palsy).
Facial cheeks (lipoatrophy in HIV therapy).
Causes & Risk Factors
Local emaciation can stem from a variety of sources. Key etiologies include:
Neurological
Nerve injury or compression (e.g., sciatic nerve palsy) leads to denervation atrophy of muscle fibers.
Peripheral neuropathy (e.g., diabetic neuropathy) may preferentially affect distal muscle groups.
Metabolic & Inflammatory
HIV‑associated lipoatrophy: Antiretroviral drugs (stavudine) can cause focal fat loss in the face and limbs.
Autoimmune myositis: Chronic inflammation leads to muscle fiber damage and localized wasting.
Mechanical & Iatrogenic
Pressure atrophy: Immobilized limbs under constant pressure (bedridden patients) lose local muscle bulk.
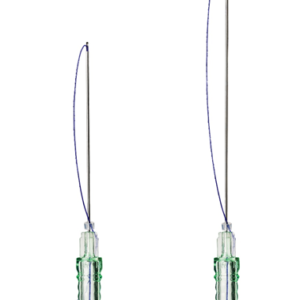
Repeated injections: Insulin or corticosteroids injected at the same site cause lipoatrophy.
Risk Factors
Prolonged immobilization
Uncontrolled metabolic disease (e.g., diabetes)
History of localized trauma or surgery
High‑dose, long‑term corticosteroid use

Clinical Presentation
Recognizing local emaciation early hinges on a detailed history and focused physical exam.
Patient Description:
“It looks like a dent in my thigh.”
Noticed after months of self‑injections or following an injury.
Signs & Symptoms:
Visible depression or thinning of the skin overlying muscle.
Palpable reduction in muscle mass.
Possible weakness or reduced range of motion if motor fibers are involved.
Visual & Palpation Findings:
Asymmetry compared to the contralateral limb.
Soft, pliable skin overlying scant subcutaneous tissue.
Muscle bulk diminished on resistance testing.
Diagnostic Workup
A structured approach ensures accurate differentiation from other wasting disorders.
History & Physical Exam
Document onset, progression, associated pain or sensory changes.
Examine for signs of systemic illness (e.g., weight loss, fevers).
Imaging
Ultrasound: Quick assessment of subcutaneous fat thickness and muscle architecture.
MRI: Gold standard for muscle volume quantification and detection of fatty infiltration.
Laboratory Tests
Inflammatory markers (ESR, CRP) for autoimmune causes.
Metabolic panel to rule out systemic malnutrition or endocrine dysfunction.
Differential Diagnoses
Cachexia (generalized wasting in chronic disease)
Sarcopenia (age‑related muscle loss)
Focal lipodystrophy (e.g., Barraquer‑Simons syndrome)
Neoplasm (rarely, localized malignancy)
Management Strategies
Treatment hinges on addressing underlying causes and restoring tissue volume.
Rehabilitative Therapy
Physical Therapy & Exercise
Targeted resistance training to stimulate muscle hypertrophy.
Electrical muscle stimulation in denervated fibers.
Occupational Therapy
Adaptive equipment for patients with functional impairment.
Nutritional Support
Dietary Optimization
High‑protein diet (1.2–1.5 g/kg/day) to support muscle synthesis.
Supplementation with leucine or HMB in severe cases.
Micronutrients
Vitamin D and calcium for muscle and bone health.
Omega‑3 fatty acids to modulate inflammation.
Medical Treatment
Pharmacotherapy
Low‑dose corticosteroids for inflammatory myopathies.
Anabolic agents (e.g., testosterone) in selected hypogonadal patients.
Biologics
In refractory autoimmune cases, agents like rituximab may be considered.
Surgical & Aesthetic Interventions
Fat Grafting (Autologous)
Harvesting fat from uninvolved sites to fill depressed areas.
Long‑term viability with proper technique.
Implants & Fillers
Silicone implants in muscle cavities.
Hyaluronic acid fillers for small defects.
Monitoring & Follow‑Up
Regular assessment of muscle girth and strength.
Repeat imaging at 6–12 months to evaluate tissue restoration.
Adjust therapies based on response.

Prevention & Patient Education
Empowering patients with preventive strategies reduces recurrence:
Injection‑Site Rotation:
Alternate sites every injection to avoid lipoatrophy.
Pressure Relief & Positioning:
For immobilized patients, reposition every 2 hours; use specialized mattresses or cushions.
Early Mobilization:
Initiate physical activity as soon as medically feasible post‑injury or surgery.
Lifestyle Modifications:
Smoking cessation, moderate alcohol intake, and weight management to support tissue health.
Prognosis & Outlook
Recovery from local emaciation varies by cause and timeliness of intervention:
Favorable Factors:
Early detection and rehabilitation.
Reversible etiologies (e.g., injection‑related lipoatrophy).
Chronicity & Complications:
Long‑standing denervation may lead to irreversible fatty infiltration.
Psychological impact from cosmetic deformity; referral to counseling services may be warranted.
Conclusion & Call to Action
Local emaciation—though limited in distribution—can substantially impair function and self‑image. By understanding its multifactorial causes, executing a thorough diagnostic workup, and implementing targeted rehabilitative, nutritional, and procedural therapies, clinicians can optimize outcomes.
If you or someone you know is experiencing unexplained thinning in a specific body area, consult a neurologist or physiatrist promptly. Early intervention not only restores lost tissue but also prevents long‑term complications. For more on related topics, explore our muscle wasting and sarcopenia resources.